
Source: Supra-Gingival Minimally Invasive Dentistry: A Healthier Approach to Aesthetic Restorations, published by Wiley-Blackwell
What Is Occlusal Disease?
Disease is defined as an “abnormal condition of an organism as a consequence of infection, inherent weakness or environmental stress, that impairs normal physiological function.” While negative effects of occlusion have typically been referred to as “problems or conditions,” based on the definition provided, the disease is a more appropriate term, as it is an abnormal condition, it is pathological, and it causes dysfunction.
To be more specific, occlusal disease is a generic term donating any destructive process evident in any part of the masticatory apparatus (joint, muscles, periodontium or teeth), as a consequence of occlusal disharmony and/or parafunction.

Figure 1

Figure 2
This picture above tells a big story. These two patients are both the same age – in their early 30s. The difference is that the patient in Figure 1 has a healthy mouth and the patient in Figure 2 has a very aggressive type of occlusal disease.
Why Should We Treat Occlusal Disease?
Regardless of the obstacles, treating occlusal disease is crucial, because for every single dentist, everything we do affects occlusion and occlusion affects everything we do.
We see the effects of occlusal disease every day. Ceramic restorations are at an increased risk when a patient suffers from traumatic occlusion combined with parafunctional activity (occlusal disease). [1] Because of the fear of fractured restorations, many dentists cut crowns, rather than use partial coverage.
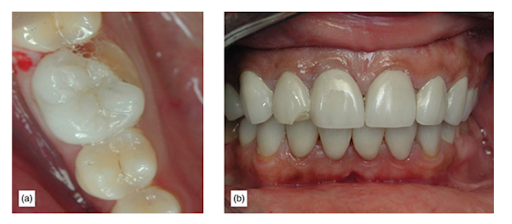
- (a) Fractured onlay. (b) Fractured veneers.
Parafunctional activity combined with a traumatic bite (occlusal disease) is the cause of restoration failures[2], and good occlusal management can lead to success in other cases. So it is important for us to manage this problem and to educate our patients so they are aware that they have this condition, and so we can do healthier, supragingival minimally invasive dentistry.
If we treated occlusal disease routinely in all of our patients and managed occlusion, many of our problems would go away.
Understanding occlusion and occlusion management:
- Allows for better diagnosis in complicated cases, due to undiagnosed occlusal problems being responsible for many catastrophic treatment decisions.
- Encourages healthier, more supragingival minimally invasive dentistry.
- Permits better, more comprehensive treatment for patients. Fear of fractures prevents dentists from undertaking single-tooth dentistry and encourages the avoidance of more comprehensive cases.
- Provides a healthier dental life for patients with occlusal disease. through early diagnosis and minimally invasive management.
- Opens up a large generator of production because there are many patients with occlusal disease that need treatment for occlusal disease.
Good occlusal management can lead to success in even difficult cases.


- (a) Severely worn dentition. (b) A 15-year postoperative image of porcelain veneers with Noritake feldspathic porcelain. (c) The patient needs aesthetic treatment. (d) Traumatic occlusion, which can lead to failure of any restoration. (e) Finished aesthetic rehabilitation using Noritake feldspathic porcelain veneers. (f) Restorative correction of the cross-bite using porcelain veneers. (g) Canine guidance to manage forces. (h) 3-years postoperatively.
Why Occlusal Disease Often Goes Untreated
There are millions of patients with severe occlusal disease that go untreated[3]. A primary obstacle for clinicians in managing occlusal disease is the patient’s disinterest in their bite or accepting the importance of wearing a night guard. In addition to this, is the clinician’s failure to explain to the patient that there are more damaging signs and symptoms occurring, and how occlusal disease is not just wear.
Another major obstacle is the erroneous idea that the best way of managing worn dentition is extensive rehabilitation. Occlusal management can be and should be minimally invasive.
The first step managing occlusal disease is the implementation of a simple, yet effective system for accomplishing early diagnosis, the Occlusal Disease Management System [4].
Occlusal Disease Management System
Stage 1: Initial Occlusal Evaluation
The first stage of the occlusal disease diagnosis system is occlusal screening, which shouldn’t take long.
Our dental auxiliary team should be in charge of educating and motivating our patients. They should spend a certain amount of time educating our patients about occlusal disease, in addition to the other diseases that affect our patient’s dentition. Then they are in charge of taking the necessary records, which are incredibly important, in preparation for us to do a comprehensive examination as we do routinely.
The next step would be to have a conversation with our patient about their dental history. This is useful to get to know the patient’s dental IQ and get to know if the patient has symptoms already that they are aware of.
Once we are finished reviewing the patient’s dental history with the patient, then we are ready to do our comprehensive examination. And as you know, a comprehensive examination should include the diagnosis of caries, the diagnosis of periodontal disease, and certainly the diagnosis of occlusal disease.
We already started diagnosing occlusal disease because when we went over the dental history, we looked at some of those questions that are specifically targeted so we can start finding out if the patient is aware that they have certain signs and symptoms of occlusal disease. And sometimes when we discuss the symptoms with the patients, they are surprised that this is even related to their bite.
The Seven Signs and Symptoms of Occlusal Disease
There are seven signs and symptoms of occlusal disease. If the patient has any of these or suffers from any of these signs or symptoms, then they do have an occlusal disease to a certain degree.
The seven signs and symptoms are:
- Pathological tooth wear, chipping, or fractures
- Tooth hypersensitivity
- Tooth hypermobility
- Fremitus
- Abractions
- Severe localized bone destruction
- Muscle pain and TMJ pain
Next Steps
After the first stage of diagnosis, it is time to allow the patient to make some choices. We can certainly offer our patients the basic dental treatment that they need, which may be the treatment of periodontal disease, broken fillings, and other things that they might have. But we should also offer the patient to treat the occlusal disease.
For us to treat occlusal disease, we would need to do a more comprehensive occlusal and TMJ examination, which is phase two. So far, we have finished stage one of the occlusal disease diagnosis system. Now we are able to assess that the patient has occlusal disease and inform them.
If they refuse advanced evaluation, we must accept that we have done our part in informing the patient that they have a disease that is destroying their teeth and that some of their restorations may have a shorter lifespan due to this disease. We have planted a seed in their mind that may allow them to reconsider in the future.
If the patient does accept additional examinations, stage 2 and 3 should proceed.
Stage 2: Occlusal and TMJ Examination (as needed and accepted by patients)
Stage 2 is for patients with moderate to severe signs/symptoms, those who wish aesthetic rehabilitation, or need extensive restorative dentistry and are motivated to pay for a complete occlusal analysis with mounted casts.
Stage 3: TMJ Examination or Referral to Local Expert
Stage 3 is for patients diagnosed with true joint disease or TMD. This usually means referral to a specialist or if the clinician is trained to treat those cases, treatment.
We hope this article was valuable to you. Our mission is to provide proven, real-world practical techniques, resources, articles and videos to help the community of caring dentists, who value the benefits of minimally invasive Supra-gingival dentistry, expand their knowledge and achieve clinical success, thus giving their patients a healthier form of dentistry.
If you want to delve deeper into Occlusion and learn how to develop a restorative diagnosis while implementing an occlusal strategy, come join us for our next Occlusion workshop. For updates on newly published articles, courses, and more, sign up for the Ruiz Dental Seminars Newsletter.
Sources:
- Van Dijken JW, Hasselrot L. A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater, 2010; 26(9): 929-923.
- Ekfeldt A, Karlsson S. Changes of masticatory movement characteristics after prosthodontic rehabilitation of individuals with extensive tooth wear.
- Christensen GJ. Abnormal occlusion conditions: A forgotten part of dentistry. J Am Dent Assoc, 1995; 126(12): 1667-1668
- Ruiz JL. Coleman TA. Occlusal Disease Management System. The Diagnosis Process. Compendium 2008 Vol. 29 No. 3
Los Angeles Institute of Clinical Dentistry & Ruiz Dental Seminars Inc. uses reasonable care in selecting and providing content that is both useful and accurate. Ruiz Dental Seminars is not responsible for any damages or other liabilities (including attorney’s fees) resulting or claimed to result in whole or in part, from actual or alleged problems arising out of the use of this presentation. The techniques, procedures and theories on this presentation are intended to be suggestions only. Any dental professional viewing this presentation must make his or her own decisions about specific treatment for patients.

