The key to implementing supra-gingival dentistry, is the use of translucent restorative materials to allow for a nice esthetic blend of the restorative margin, thus allowing us to leave the margins above the gum.
Available Paradigm-shifting Dentistry Workshops
That is easier when teeth have normal, or ideal color. Darker teeth benefit from the use of pre-prosthetic bleaching, using good quality bleaching systems like Venus White (Kulzer).
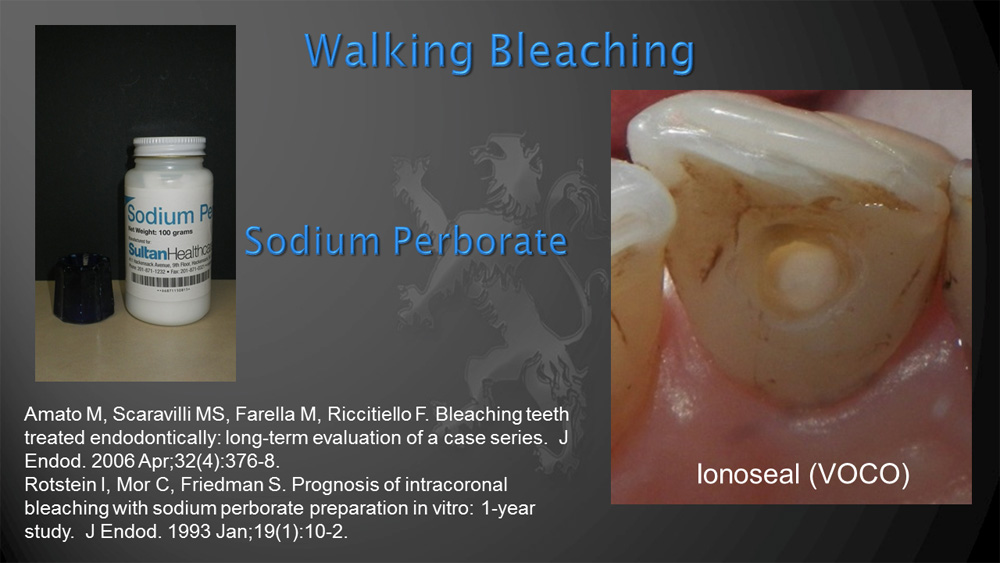
Some endodontically treated teeth may be considerably darker than the adjacent teeth. The traditional approach is to deal with this issue by placing an opacious full coverage crown with subgingival margins to hide the color difference, with all the disadvantage previously discussed. Internal bleaching, or walking bleaching, is a desirable alternative to the more destructive crown option. Internal bleaching has been shown to be successful, durable and safe.[i] [ii] Rotstein and others have shown that sodium perborate has been found to be as effective as hydrogen peroxide with a suggested decrease chances of oxidative irritation and root resobtion. [iii] [iv]
Additionally because endodontically treated teeth may have a tendency to become dark over time, sometime more tooth preserving techniques like porcelain veneers are not performed to avoid the possibility of tooth darkening. Tooth color changes can be minimized by properly cleaning the pulp chamber of pulp remnants and endodontic filling materials.[v] In cases where teeth become darker in time, internal bleaching can also be performed even years after porcelain veneer are placed. The following is Rotstein’s walking bleaching technique:
- Familiarize the patient with the possible causes of discoloration, the procedure to be followed, the expected outcome, and the possibility of future rediscoloration.
- Radiographically assess the status of the periapical tissues and the quality of endodontic obturation. Endodontic failure or questionable obturation should always be retreated prior to bleaching.
- Assess the quality and shade of any restoration present and replace it if defective. Tooth discoloration is frequently the result of leaking or discolored restorations. In such cases, cleaning the pulp chamber and replacing the defective restorations will usually suffice.
- Evaluate tooth color with a shade guide and, if possible, take clinical photographs at the beginning of and throughout the procedure. These provide a point of reference for future comparison.
- Isolate the tooth with a rubber dam. The dam must fit tightly at the cervical margin of the tooth to prevent possible leakage of the bleaching agent onto the gingival tissue. Interproximal wedges and ligatures may also be used for better isolation.
- Remove all restorative materials from the access cavity, expose the dentin, and refine the access. Verify that the pulp horns and other areas containing the pulp tissue are clean. Remove all materials to a level just below the labial–gingival margin.
- To cover the endodontic obturation, apply a sufficiently thick layer, at least 2 mm, of a protective white cement barrier, such as polycarboxylate cement, zinc phosphate cement, glass ionomer, intermediate restorative material (IRM), white colored MTA or Cavit. The coronal height of the barrier should protect the dentinal tubules and conform to the external epithelial attachment.
- Prepare the walking bleach paste by mixing sodium perborate and an inert liquid, such as water, saline, or anesthetic solution, to a thick consistency of wet sand. Although sodium perborate plus 30% H2O2 mixture may bleach faster, in most cases, long-term results are similar to those with sodium perborate and water alone and therefore need not be used routinely. With a plastic instrument, pack the pulp chamber with the paste. Remove excess liquid by tamping with a cotton pellet. This also compresses and pushes the paste into all areas of the pulp chamber.
- Remove the excess bleaching paste from undercuts in the pulp horn and gingival area and apply a thick well-sealed temporary filling (preferably IRM) directly against the paste and into the undercuts. To ensure a good seal, carefully pack the temporary filling, at least 3 mm thick.
- Remove the rubber dam and inform the patient that bleaching agents work slowly and that significant lightening may not be evident for several days.
- Evaluate the patient 2 weeks later and, if necessary, repeat the procedure several times. Repeat treatments are similar to the first one.
- As an optional procedure, and in limired cases, if initial bleaching is not satisfactory, strengthen the walking bleach paste by mixing sodium perborate with gradually increasing concentrations of H2O2 (3% to 30%) instead of water. Start with low concentrations. As low as possible and practical. The more potent oxidizers may have an enhanced bleaching effect but should not be used routinely because of the possibility of permeation into the tubules and damage to the cervical periodontium by these more caustic agents. In such cases, a protective cream, such as Orabase or Vaseline, must be applied to the surrounding gingival tissues prior to dam placement. In most cases, discoloration will improve after 1 to 2 treatments. If after three attempts there is no significant improvement, reassess the case for correct diagnosis of the etiology of discoloration and treatment plan.
References
[i] Amato M, Scaravilli MS, Farella M, Riccitiello F. Bleaching teeth treated endodontically: long-term evaluation of a case series. J Endod. 2006 Apr;32(4):376-8.
[ii] Rotstein I, Mor C, Friedman S. Prognosis of intracoronal bleaching with sodium perborate preparation in vitro: 1-year study. J Endod. 1993 Jan;19(1):10-2.
[iii] Rotstein I, Zalkind M, Mor C, Tarabeah A, Friedman S. In vitro efficacy of sodium perborate preparations used for intracoronal bleaching of discolored non-vital teeth. Endod Dent Traumatol. 1991 Aug;7(4):177-80.
[iv] Palo RM, Valera MC, Camargo SE, Camargo CH, Cardoso PE, Mancini MN, Pameijer CH. Peroxide penetration from the pulp chamber to the external root surface after internal bleaching. Am J Dent. 2010 Jun;23(3):171-4.
[v] Plotino G, Buono L, Grande NM, Pameijer CH, Somma F. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008 Apr;34(4):394-407.

