
Source: Supra-Gingival Minimally Invasive Dentistry: A Healthier Approach to Aesthetic Restorations, published by Wiley-Blackwell
For clinicians who are passionate about minimally invasive dentistry, understanding occlusal management can encourage healthier, more supragingival minimally invasive dentistry because the fear of fractured restorations often forces the dentist to cut crowns rather than use partial coverage.
The Occlusal Disease Management System is incremental, based on severity, and incorporates a patient’s willingness to accept diagnosis and treatment. It allows even the busiest of dentists to incorporate occlusal diagnosis and therapy for every patient, as it only takes 3 minutes to do a simple occlusal diagnosis.
Knowing the seven signs and symptoms of occlusal disease is part of the first stage of the occlusal disease management system, aiding in diagnosis. Every patient in the practice must have an occlusal examination as part of a comprehensive examination, as well as periodic examinations.
The Seven Signs and Symptoms of Occlusal Disease
When a patient presents with one or more of the seven signs and symptoms, it can be assumed the patient has occlusal disease, and, depending on the severity, a course of treatment will be suggested.
If the patient does not display any signs or symptoms, it is safe to assume that they are well adapted to their occlusion, have no pathology, and do not need occlusal management.
1. Pathological Tooth Wear, Chipping, or Fractures.

Figure 1: Multiple chips on posterior teeth.
The first sign and symptom of occlusal disease. is pathological tooth wear, chipping, and fractures.
This is simple for us to assess by a visual examination of the teeth, and should only take seconds.
We only need to look at our patient’s teeth, and we can see if the patient’s teeth are worn beyond the point that they should be. Multiple chips or small and large fractures on the teeth and restorations are indicators that the patient is suffering from pathological occlusion. Identifying the severity of the condition is also important and it is also dependent on the age of the patient. When severe wear is present, restorative treatment should be attempted. However, early diagnosis and management are preferable to waiting until serious damage is present.
2. Cervical Dentin Hypersensitivity.
Cervical dentin hypersensitivity is one of the most common signs of occlusal disease. Patients come in daily with sensitivity issues, such as sensitivity to hot and cold. They sometimes feel that the sensitivity is on one side at one point and the other side at another time.
Tooth hypersensitivity is multifactorial, and the etiology is often debated in the literature, ranging from gingival recession and root exposure to acidic foods and improper brushing as some of the factors. Hypersensitivity is still mostly treated with desensitizing toothpaste and topical agents, with very limited and temporary success, and with restorations, with equally short-term success.
Considerable controversy exists about the role of occlusion on hypersensitivity [1]. A number of studies that discredit the role of occlusion often lack a good method for diagnosing occlusal issues or a treatment approach, rendering their findings inconclusive [2]. Experienced clinicians understand that occlusal trauma can cause sensitivity, even severe sensitivity.
In a three-part clinical study, Coleman and colleagues found that occlusal trauma was the primary source of cervical dentin hypersensitivity, and that occlusal adjustment was the best modality for a long-term resolution [3].
My extensive clinical experience in diagnosing tooth hypersensitivity and occlusive disease, and treating it with occlusal therapy, agrees with Coleman’s findings.

Figure 2: Three overhanging class V fillings to treat sensitivity; 1 year later, the patient still has severe sensitivity.
3. Hypermobility.
The next sign of occlusal disease is tooth hypermobility. In cases where the degree of tooth mobility exceeds what is expected given the level of attachment and bone support, we can say that the tooth has hypermobility. Therefore, when a patient exhibits a mobility level of 2, 3, or even 4 in a tooth, despite having a satisfactory attachment level and solid bone support, this is an indicator of occlusal interference and occlusal trauma.
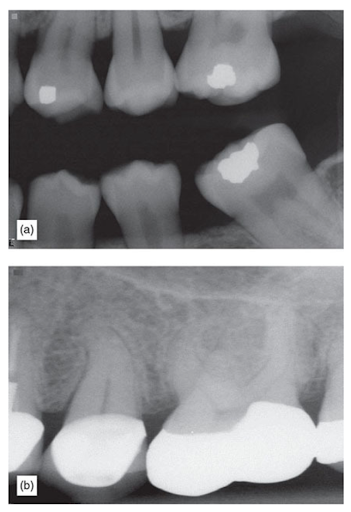
Figure 3: (a) A lower second molar having acceptable periodontal support, but severe mobility. (b) A tooth with acceptable periodontal support but severe mobility; sometimes the periodontal ligament is widened, but sometimes it is not.
4. Fremitus.
The next sign of occlusal disease is Fremitus. Feminus is the mobility of the anterior teeth, usually a violation of the envelope of function. It can be tested by the clinician placing their finger on the front teeth of the patient and asking them to tap their teeth together. If there is movement on any of those front teeth as they are tapped together, that would be a sign that there is an envelope of function violation. The consequences of the untreated occlusal trauma which causes fremitus are proximal contact opening and teeth separating, broken incisal edges, broken incisor restorations and fractured teeth.

Figure 4: Tooth with fremitus.
5. Abfractions (Non-Carious Cervical Lesions).
Abfractions are quite controversial in dentistry. A more popular term today is non-carious cervical lesions” (NCCL). Nevertheless, the term abfraction denotes its occlusal origin. Many dentists believe that NCCL is caused by brushing or abrasive toothpaste. While NCCL have a multifactorial etiology, including toothpaste abrasion, acidic drinks, habits and other factors, the primary cause of their formation is lateral interference, as many studies have suggested.
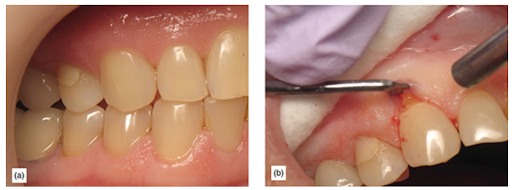
Figure 5: (a) This tooth has a subgingival abfraction, not caused by toothpaste abrasion. (b) Using a gingival retractor, the abfraction becomes evident; this patient had group function and was a heavy bruxer.
6. Severe Localized Bone Destruction, Secondary to Periodontal Disease.
The next sign of occlusal disease is severe localized bone destruction, secondary to periodontal disease. For example, a full-mouth x-ray may reveal the presence of periodontal disease throughout their entire dentition, with only one or few teeth with severe bone loss. of teeth in a patient. An often overlooked factor contributing to accelerated bone loss, as the existing literature points out, is occlusal trauma in secondary to periodontal disease. Most periodontists recognize that there is an increase in success with periodontal procedures when occlusion is considered.
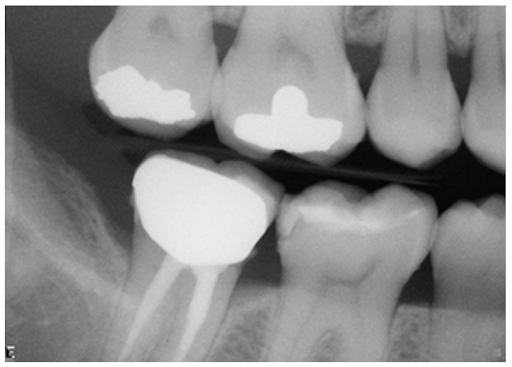
Figure 6: X-ray showing accelerated bone loss around a single tooth.
7. Muscle and Temporomandibular Joint Pain.
Pain associated with occlusal problems is a powerful motivator for treatment. Apart from wear, it is the most recognizable and obvious symptom of occlusal disease. Conversely, patients may exhibit severe headaches and pain and never link it to their dentition. This is why it is important to have a methodical system where the right questions are asked to prompt the disclosure of a symptom that the patient otherwise would not feel the need to disclose to their dentist, like headaches or migraines. While muscle pain and temporomandibular disorder have a controversial etiology, and many suggest that it has no link to occlusion, clinical experience shows otherwise. [4,5]
Course of Action
Early diagnosis and good knowledge of proper minimally invasive occlusal management can improve the quality of the patient’s dental life, as well as give clinical confidence in treatment success. Of course, the clinician’s goal is to treat every disease we are presented with, but the patient must first allow us to do so. Education is key, but if after proper education the patient is reluctant to accept that a problem exists or to accept treatment, it is acceptable to continue to treat such patients with some modifications. The patient should be informed that just as their natural teeth are suffering and wearing excessively, any restoration we place will have a tougher life and may have a shorter durability.
We hope this article was valuable to you. Our mission is to provide proven, real-world practical techniques, resources, articles and videos to help the community of caring dentists, who value the benefits of minimally invasive Supra-gingival dentistry, expand their knowledge and achieve clinical success, thus giving their patients a healthier form of dentistry.
If you want to delve deeper into Occlusion and learn how to develop a restorative diagnosis while implementing an occlusal strategy, come join us for our next Occlusion workshop. For updates on newly published articles, courses, and more, sign up for the Ruiz Dental Seminars Newsletter.
Sources:
- Cunha-Cruz J, Wataha JC, Heaton LJ, Rothen M, Sobieraj M, Scott J, Berg J; Northwest Practice-based Research Collaborative in Evidence-based DENTistry. The prevalence of dentin hypersensitivity in general dental practices in the northwest United States. J Am Dent Assoc, 2013; 144(3): 288-296.
- Senna P, Del Bel Cury A, Rosing C. Non-carious cervical lesions and occlusion: a systematic review of clinical studies. J Oral Rehabil, 2012; 39(6): 450-462.
- Coleman TA, Grippo JO, Kinderknecht KE. Cervical dentin hypersensitivity: Part III: Resolution following occlusal equilibration. Quintessence Int, 2003; 34: 427-434.
- Sipila K, Ensio K, Hanhela H, Zitting P, Pirttiniemi P, Raustia A. Occlusal characteristics in subjects with facial pain compared to a pain-free control group.
- Komazaki Y, Fujiwara T, Ogawa T, Sato M, Suzuki K, Yamagata Z, Moriyama K. Association between malocclusion and headache among 12-to-15-year-old adolescents: A population-based study. Community Dent Oral Epidemiol, 2014; 42(6): 572-580.
Los Angeles Institute of Clinical Dentistry & Ruiz Dental Seminars Inc. uses reasonable care in selecting and providing content that is both useful and accurate. Ruiz Dental Seminars is not responsible for any damages or other liabilities (including attorney’s fees) resulting or claimed to result in whole or in part, from actual or alleged problems arising out of the use of this presentation. The techniques, procedures and theories on this presentation are intended to be suggestions only. Any dental professional viewing this presentation must make his or her own decisions about specific treatment for patients.

