Source: Supra-Gingival Minimally Invasive Dentistry: A Healthier Approach to Aesthetic Restorations, published by Wiley-Blackwell
As any clinician who values minimally invasive dentistry understands, it is always preferable to retain a supragingival margin and preserve tooth structure to make restorative dentistry healthier.
However, the recommendations for bonded onlays/onlay preparation have traditionally been for simple cases that fulfill strict requirements, such as acceptable tooth color, sufficient tooth structure available, ideal location in the arch, ideal occlusion, and existing supragingival margin.
With these strict recommendations in place, research shows that more than 95% of teeth needing indirect restorations ends up being prepared for full crowns.
While less damaged teeth should be repaired with direct composite restorations, indirect restorations should be reserved for badly damaged and weakened teeth.
Expected outcomes will vary depending on the amount of remaining tooth, extension of the caries, old restorative material or fracture, and other circumstances. Modifications and different types of preparations and restorations should be considered due to these reasons.
There are three major categories in which posterior teeth requiring indirect restorations can be divided.
First Onlay Preparation Category: Simple Partial and Full Coverage on Vital Teeth
Direct restorations would not be indicated in cases where one or more of the cusps are undermined, fractured or missing, and must be onlayed.
There are simple cases in which the ideal natural tooth color and the amount of remaining tooth structure, especially the periphery of the enamel is sufficient, the final preparation is 2 mm or more from the pulp, and the existing margins are supragingival.
The supragingival protocol would allow the margins to remain supragingival without dentin sealing or buildups needed.
While most experts recommend bonded onlays for these cases, they are currently usually treated with full crowns.
Simple onlay preparation is also well suited for full mouth rehabilitation.
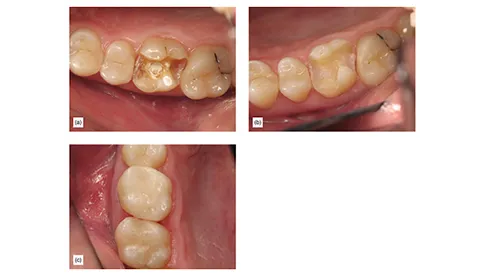
There are some experts who consider severe occlusal wear a contraindication to bonded onlays, bonded onlays in patients with severe occlusal wear have shown excellent results (Figure 1).
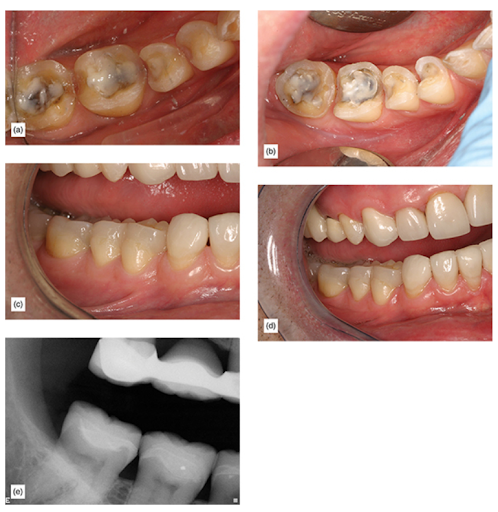
Figure 1: (a) Full lower rehabilitation with onlays and veneers. (b) Onlay preparation. (c) Finished restoration (d) restoration 3 years postoperatively (e) eight-year postoperative x-ray.
Second Onlay Preparation Category: Complex Partial and Full Occlusal Coverage Requiring Buildups on Vital Teeth
Vital teeth that are badly damaged may necessitate dentin sealing and some type of buildup, such as where the caries is very close to the pulp, where there are significant undercuts and a weakened cusp or cusps that need reinforcement, when the caries is deep at the cervical margin, and where enamel margin preservation or margin elevation techniques are needed. (Figure 2)
As these teeth are vital, color is typically not a concern. Traditionally, crowns have been recommended for such cases. However, advancements in adhesion and materials, along with the adoption of a supragingival protocol, have made it possible to achieve successful outcomes with partial coverage supragingival restorations.

Figure 2: (a) This badly damaged tooth needed onlay using caries detector to preserve as much tooth as possible and a supragingival margin. (b) After buildup and dentin sealing. (c) The finished onlay.
Third Onlay Preparation Category: Complex Full Coverage on Endodontically Treated Teeth or Teeth With Vertical Fractures
Teeth afflicted with vertical fractures, cracked-tooth syndrome, or those that have undergone endodontic treatment can and should be treated with partial coverage bonded onlays. The literature indicates an increased risk of failure for these teeth, necessitating modifications to the preparation. This may involve the addition of buildups or “margin elevation.” Depending on the dental arch and the anticipated forces, stronger restorative materials such as zirconia may be indicated.
To ensure the restorative material’s sufficient strength, a slight increase in occlusal reduction is required. Reduction should be a minimum of 2.5 mm final occlusal thickness for lithium disilicate, which is ideal for esthetically demanding premolars. It should be 2mm minimum final occlusal thickness for zirconia, which is ideal for teeth which must resist higher forces and have lower esthetic demands, such as second molars.
Increased thickness of the restorative material has been shown in clinical and finite-element studies to decrease the risk of fracture. Such teeth have traditionally been indicated for traditional full crowns. These teeth usually have large amounts of tooth missing. In teeth that are already in a very weak state, it’s counterintuitive to further remove large amounts of tooth to prepare the axial walls for mechanical retention. Because of this, supragingival minimally invasive bonded onlay restoration is the best option (Figure 3).
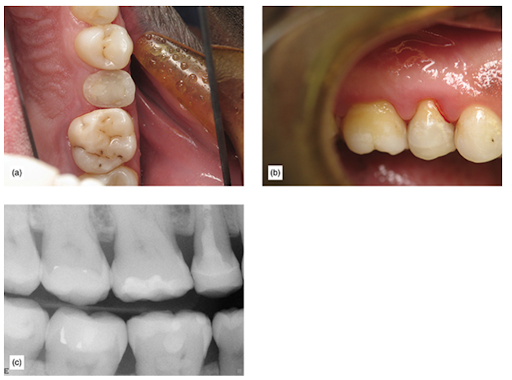
Figure 3: (a) Root canal after buildup. (b) Immediately after cementation. (c) Successful onlay 7 years postoperatively.
We hope this article was valuable to you. Our mission is to provide proven, real-world practical techniques, resources, articles and videos to help the community of caring dentists, who value the benefits of minimally invasive Supra-gingival dentistry, expand their knowledge and achieve clinical success, thus giving their patients a healthier form of dentistry.
For updates on newly published articles, courses, and more, sign up to the Ruiz Dental Seminars newsletter.
Los Angeles Institute of Clinical Dentistry & Ruiz Dental Seminars Inc. uses reasonable care in selecting and providing content that is both useful and accurate. Ruiz Dental Seminars is not responsible for any damages or other liabilities (including attorney’s fees) resulting or claimed to result in whole or in part, from actual or alleged problems arising out of the use of this presentation. The techniques, procedures and theories on this presentation are intended to be suggestions only. Any dental professional viewing this presentation must make his or her own decisions about specific treatment for patients.

